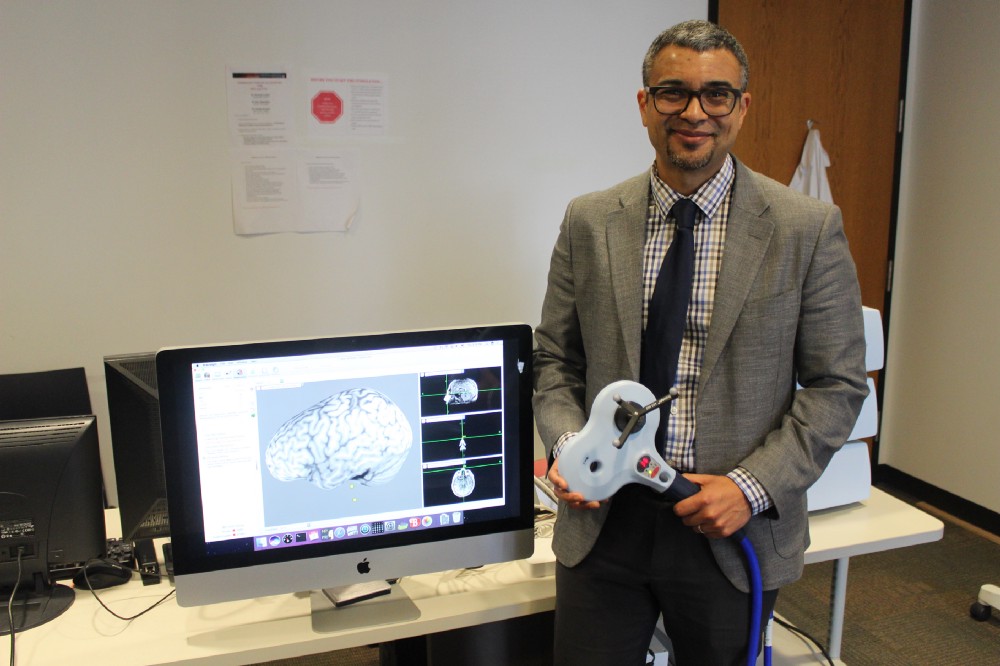
This month ANA talked to Dr. Roy Hamilton, Associate Professor at the University of Pennsylvania in the Neurology and Physical Medicine and Rehabilitation Departments and Director of both the Laboratory for Cognition and Neural Stimulation (LCNS) and the Penn Brain Science, Translation, Innovation, and Modulation (brainSTIM) Center. Dr. Hamilton discusses his work with noninvasive neuromodulation, his team’s work at brainSTIM, and more.
What does the public need to understand about noninvasive brain stimulation that it often doesn’t understand?
The single most common question I'm asked by people who are unfamiliar with brain stimulation when I first start talking about it, is whether or not techniques like Transcranial Magnetic Stimulation (TMS) and Transcranial Direct Current Stimulation (tDCS), are the same as Electroconvulsive Therapy (ECT), or as some people in the in the public refer to it, ‘electroshock therapy,’ rather inaccurately.
To me, that reflects a couple of misconceptions. The first one is actually about ECT, because often, when people are asking me that question, what they're actually asking me is a question about how dangerous they should perceive noninvasive brain stimulation as being. They are asking me to compare it to ECT because their expectation is that ECT is quite dangerous, often misinformed by the stigma that's been placed upon it in the media and entertainment. So that's often the first misconception when they're asking me that question.
The second misconception has to do with the thing they're really trying to get at, which is a fear that noninvasive brain stimulation techniques like TMS and tDCS are themselves unsafe. While I’ve already touched on the fact that ECT is generally safe, let me emphasize that the intensities of stimulation that we give with these technologies are orders of magnitude less than ECT. And so, when delivered within known, established safety parameters, TMS is a safe technology. Furthermore, there is no known history of serious adverse events with tDCS; that technology is very safe.
So, the primary misconception about these technologies stems from fear about stimulating the brain and what harm it could do to. That's the main misconception I have to get past with people.
How are treatment options for noninvasive brain stimulation different today from 10 years ago?
In 2008, noninvasive neuromodulation of the brain was approved by the FDA for its first clinical indication, which was the treatment of medication-resistant major depression. Since then, its use has certainly broadened both in terms of its application for depression—it's become much more commonplace and is offered in several clinical settings now—and the number of indications for which it is applied, or which it is approved, is also increasing. Noninvasive neuromodulation of the brain may be applied to other psychiatric conditions like Obsessive Compulsive Disorder as well as well as neurologic conditions like migraines. There is, for example, a TMS device that is approved for self-application by patients at the onset of a migraine to abort headaches. More importantly, what has really exploded over the course of the last 10 years is the number of areas in which brain stimulation is being explored as a possible clinical intervention. Areas of investigation include other neuropsychiatric and neuropsychological conditions (i.e., ADHD), chronic pain, Parkinson’s disease, cognitive and motor symptoms after a stroke, and aspects of dementia. As a consequence, there are a number of conditions for which noninvasive neuromodulation will likely be approved in the future.
What promising research is poised to change the standard of treatment for noninvasive brain stimulation?
We’re always making improvements with things like brain imaging and analyses of the data that we're getting from the brain. As those refinements become sharper, we get better information about where we ought to be going when we stimulate the brain. If you think about it, when it comes to stimulating the brain, if you don't know where to go, it doesn't matter what you can do when you get there. As our understanding of the brain grows, it tells us more and more about where we ought to be going and what we should be doing there. Improvement and refinement in technology, paired with our increasing understanding of the brain, allow us to image, target, and make predictions about specific areas that do specific things.
Another area that is poised for change is the development of new technologies, including new categories of noninvasive neuromodulation beyond magnetic and electrical stimulation. For example, Transcranial Focused Ultrasound (tFUS) allows one to use ultrasonic waves to manipulate neural activity focally and reversibly both at the surface of the brain and in structures deep in the brain’s interior. Researchers are also exploring whether different wavelengths of light could be used transcranially to manipulate brain activity. Other stimulation and modulation approaches are being explored as well. Ten years from now, noninvasive brain stimulation may not simply refer to one or two approaches, but might instead represent a whole toolbox of techniques that can be applied flexibly for different medical indications, different areas of the brain, and different effects.
What work is your lab undertaking to move the understanding of noninvasive brain stimulation forward?
There's a common theme shared among a number of investigators in our center, myself included, even though we're investigating different disorders, diseases, and processes: the notion that if one had a better understanding of the critical connections of the brain that enable normal cognitive functions and are implicated in specific diseases of cognition and neural function, one would be better able to target brain stimulation more precisely. Many of us share the common objective of exploring how individual brains differ from one another patient in terms of their connectivity, and how that connectivity relates both to neurological symptoms and optimal stimulation approaches to treatment. Whether we're talking about investigators in my group who are psychiatrists and looking at this in the context of psychiatric disorders, like depression, OCD, or ADHD, or we’re talking about neurologists like myself who are thinking about this in terms of disorders like stroke and dementia. The common thread is the idea of individualized neuromodulation—a noninvasive brain stimulation version of personalized medicine. I think achieving that is going to be an important step forward for the translation of neuromodulation into clinical spaces and also an important approach for strengthening our understanding of the organization of the brain.
How has COVID-19 affected your research on noninvasive brain stimulation?
Quite dramatically! Our research can broadly be divided into two categories.
Many of us do some form of basic cognitive neuroscience research involving healthy human subjects. This research uses noninvasive neuromodulation tools to elucidate structure-function relationships or network-function relationships in the brain as they pertain to human cognition, emotion, perception, and other neural operations. Other among us employ neuromodulation interventions in clinical research, seeking to use stimulation to enhance cognitive or behavioral outcomes in individuals with disorders of the brain and mind. All of that requires direct contact with human subjects, so you can only imagine that the initial total shutdown of our institution in the wake of the COVID-19 pandemic deeply affected our research. As we slowly start to open up again, we really have to think about how we are navigating the risks posed to our patients and to healthy subjects who we would want to bring into the laboratory. After all, brain stimulation is on some level a ‘contact sport,’ in that we physically touch the heads of our subjects. We're now thinking very carefully about how we manage issues like appropriate distancing and PPE, in order to protect our patients and ourselves. We are cautiously optimistic that we will be able to relaunch our research appropriately. Of course, our time away from the lab wasn’t totally wasted. Like many labs, when we first were shut down, we recognized that we had a large backlog of data that were waiting to be analyzed, papers that were waiting to be written, and things like that. So, we kept ourselves occupied. But we are now preoccupied with cautiously, safely, and appropriately reopening the laboratory and getting back to a new normal with respect to human subjects research.
How has the ANA supported your career and/or work in this area?
The ANA has provided a great backdrop for my career. The ANA has always been an organization within which I have been able to find supportive colleagues and mentors. It's has provided a venue where I could present my research, and now the trainees in my lab and of the Center can present the research that they're doing. Thus, as I've matured somewhat in this work, it's become useful not just for me, but also for the individuals I'm training. That's been the primary utility of the ANA, being the premier society for academic neurologists. ANA meetings create a space for frequent contact with individuals who can really help to advance one’s career, since so many fellow ANA members are themselves prominent researchers in the field with their with their own outstanding work. Overall, it's really been fantastic to be in the ANA. I recall being a medical student, when I was in a laboratory getting my first taste of brain stimulation. My research mentor at the time was being inducted as a fellow of the of the ANA. I remember going to the meetings and thinking, “This is where I want to be when I ‘grow up,’” and I am so excited that it came to fruition.
Infuse your career or department with fresh thinking with ANA’s MentorLink. Learn more at myana.org/career/mentorlink.
